Closure of a Patent Foramen Ovale after Presumed Coronary Paradoxical Embolism in Young Woman: A Case Report
Boka Benedicte Carine1*, Thebault Christophe1
Institut De Cardiologie D’abidjan, Ch De Paimpol. Université Félix Houphouët-Boigny UFR des Sciences Médicales Abidjan, Lagunes Côte d’Ivoire, Paimpol, France.
Received Date: November 14, 2018; Accepted Date: November 16, 2018; Published Date: November 27, 2018*
Corresponding author: Boka Benedicte Carine, 36 Chemin De Kerpuns 22500 Paimpol/ BP V 206 Abidjan, Institut De Cardiologie D’abidjan, Ch De Paimpol. Universite Felix Houphouët-Boigny UFR des Sciences Medicales Abidjan, Lagunes Côte d’Ivoire, Paimpol, France. Tel:+33646475824, 22507767552 ; Email: benedicteboka@yahoo.fr
Abstract
Background: One of the most common congenital heart disease is atrial septal defect. This conditions may be a symptomatic or responsible of morbidity, mortality and reducing of life expectancy. After paradoxical embolism, it is common in case of stroke to propose closure of patent foramen ovale. What about myocardial infarction in young?
Case Summary: We report the case of a young caucasian french woman without cardiovascular factor which had an acute chest pain. We diagnosed a presumed myocardial paradoxical embolism via a patent foramen ovale associated to atrial septal a neurysm. After long term oral anti coagulation, she benefits of an Amplatzer device implantation for closure of her atrial septal defect.
Discussion: After a paradoxical embolism, it is possible to introduce more aggressive thérapeutic than anticoagulation to avoid recurrence and the devastating effect of coronary heart disease and secondary effects of treatment on active young patient.
Conclusion : Risk of recurrence persists until the underlying cause is not treated and is higher in the case of ASA than in isolated FOP. More aggressive therapeutic strategy to reduce the risk of further embolism in active young patient without significant risk factor that have different prognoses than older patient could be PFO closure by Amplatzer occluder.
NB: Patient was agreed with this report.
Keyword: Myocardial Infarction; Paradoxical Embolism ; Patent Foramen Ovale
Introduction
Coronary heart disease in young patient is a big problem regarding the prognose and the choice of treatment link to etiology. We describe the case of a young woman without significant cardiovascular factor that had anterior myocardial infarction due to coronary thrombi of embolicorigin. Echocardiogram reveals a patent foramen ovale associated with an atrial septal aneurysm.
The Case
A 27-year-old woman, 2 children, who had an intrauterine device complains of acute chest pain, we discover an acute coronary syndrome with persistent ST segment elevation in stable condition (Figure 1).
 Figure 1: Electrocardigraphy showing the myocardial infarction
Figure 1: Electrocardigraphy showing the myocardial infarction
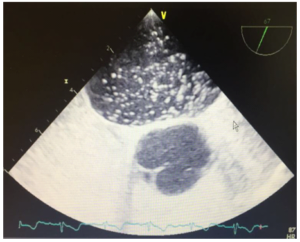
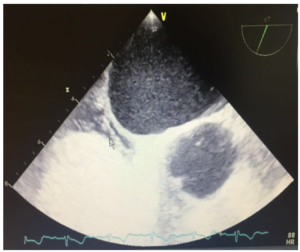
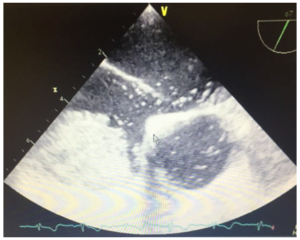
Coronary angiography revealed a single-vascular lesion with acute occlusion of the second branch of the anterior distal anterior descending artery of thrombotic appearance associated with a thrombotic occlusion of the second branch of the first diagonal and a thrombotic occlusion of the very distal part of the first diagonal. Echocardiography showed an unexpanded left ventricle, not hypertrophied with segmental disorders of contractility, the ejection fraction of the left ventricle was estimated at 45-50% without visualized thrombus. There was a septal defect in the atrial stage that motivated transesophageal echocardiography; saline bubble contrast injection allowed to show the presence of a patent foramen ovale (PFO) with significant passage at the basal state associated with an atrial septal aneurysm (ASA) without intra-cavitary thrombus visualized (Figure 2).
 (A)
(A)
 (B)
(B)
 (C)
(C)
Figure 2: Transoesophagial echocardiography showing atrial septal default.
A second control coronarography was performed 2 days later after initiation of treatment with anticoagulant, inhibitor of the conversion enzyme and beta blocker; it showed a complete reversal of the coronary axes and the disappearance of the thrombi. As part of the etiological assessment, the imaging and biological examinations were performed without particularity. The presence of thrombus in the coronary circulation and the normality of coronary arteries confirmed an embolic cause. We consider the condition as a presumed coronary paradoxical embolism. She was on oral anticoagulation with apixaban and benefit of a cardiac rehabilitation programme and ther apeutic education. Given the prognostic and potential therapeutic implications, we propose these young woman trans-catheter closure of this atrial septal defect.
Few month later, she under went amplatzerdevice implantation of a 35 mm. A manual microbubble injection test was performed at the level of the inferior vena cava showing the absence of passage right - left, the existence of a device in place without visible residual shunt, procedure performed under local anesthesia and under treatment with apixaban. She was exhaled the day after the procedure without modification of the treatment.
Discussion
Treatment of paradoxical embolisms through a PFO has been widely studied in the context of cerebrovascular accidents that constitute the most frequent clinical manifestation of presumed paradoxical embolism. The treatment is based on medical treatment to suppress the consequence or prevent recurrence and elimination of the pathway allowing paradoxical embolism. We extrapolated results in cases of non-cerebral embolic arterial accidents.
Discovering a PFO may be incidental or stroke related. To establish a link between PFO and stroke we can use the score Risk of Paradoxical Embolism (RoPE) [1]. A score RoPE up or equal to 7 (maximum score 10) relate the stroke to the PFO and allowed to have PFO closure for secondary prevention. Our patient 27 years (5), no history of hypertension (1), diabetes (1), of stroke or TIA (1), non smoker (1) had a score of 9 so at risk of further emboli [1]. Various therapeuticare available in secondary prevention: antiplatelet agents; oral anticoagulants; surgical closure and percutaneous closure of the PFO. Option should be chosen by weighting the risk of the treatment it self against the expected benefit.
Isolated PFO is a fairly common finding in practice and the risk of recurrence in the absence of associated atrial septal aneurysm (ASA) is identical to that of patients without PFO. PFO and ASA combination appears to be particularly susceptible to recurrence and is a sub group for which secondary preventionis more aggressive than antiplatelet or oral anticoagulant [2]. In facts, ASA causes atrial dys function that may promote thrombus formation in the left atrium. Closure of PFO in patients with ASA is indicated [3]. We chose Apixaban regarding results of ameta-analysis prouving that anticoagulation issuperior to aspirin, however, the risk of hemorrhage due to long-term anticoagulation remains high [4]. PFO closure indications for secondary prevention of cryptogenic stroke are: stroke recurrence under anticoagulation therapy, contraindication or refusal of anticoagulant therapy or concomitant venous thrombo embolism with high risk of paradoxical embolism recurrence. In primary prevention only platypnea orthodeoxia syndrome is indicated [5]. Recent results of 3 surveys prouve the benefits and superiority of PFO closure over medical therapy in secondary prevention of stroke [6].
Conclusion
Risk of recurrence persists until the underlying cause is not treated and is higher in the case of ASA than in isolated FOP. More aggressive therapeutic strategy to reduce the risk of further embolism in active young patient without significant risk factor that have different prognosis than older patient could be PFO closure by Amplatzer occluder.
NB: Patient was agreed with this report.
References
- Kent DM, Ruthazer R, Weimar C, Mas JL, Serena J, et al. (2013) An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology 81: 619-625.
- Almekhlafi MA, Wilton SB, Rabi DM, Ghali WA, Lorenzetti DL, et al. (2009) Recurrent cerebral is chemia in medically treated patent foramen ovale: a meta-analysis. Neurology 73:89-97.
- Dalen JE, Alpert JS Which (2018) Patent Foramen Ovales Need closure to prevent Cryptogenic Strokes? Am J Med 131: 222-225.
- Orgera MA, O’Malley P, Taylor AJ (2001) Secondary prevention of cerebral is chemia in patent foramen ovale: systematic review and meta-analysis. South Med J 94: 699-703.
- Magois VE, Aubry P, Andrejak C, Peltier M, Saidi L, Rey C, Jounieaux V (2011) Hypoxémie « On–off ». Rev MalResp 28: 668-67.
- Manolis AS (2017) Percutaneous closure of Patent Foramen Ovale for cryptogenic Stroke : The issue is finally settled. Rhythmos: october 12: 4.
Citation: Boka BC, Christophe T (2018) Closure of a Patent Foramen Ovale after Presumed Coronary Paradoxical Embolism in Young Woman: A Case Report. Inte Jr Cardiac Scie and Res: IJCSAR-107.
