The Effects Of A Dynamic Apparel Technology On Scapular Kinematics And Muscle Activity
Seiya Liu1, David Matsumura MD2*, Jeremee Bornstein3, Imon Rahaman4, Seiji Liu5, Bryan Li5, James Lin DDS6, Mika Liu7, Earl Brien MD2
1Harvard University, Cambridge, MA, USA
2Cedars-Sinai Medical Center, Los Angeles, CA, USA
3Tufts University, Dept of Biomedical Engineering, Medford, MA, USA
4Massachusetts Institute of Technology, Cambridge, MA, USA
5IFGFIT, Los Angeles, CA, USA
6Sherman Oaks Smile Center, Sherman Oaks, CA, USA
7Stanford University, Stanford, CA, USA
Abbreviations
Ergonomics, FIT, IFGFIT, Integrated Garment Technology, Kyphosis, Musculoskeletal Disorders (MSDs), Neck and Back Pain, Posture Recovery thoracic mobility, PPR tech, Scapular Alignment, Scapular kinematics, Surface Electromyograph (sEMG)
Keywords: Posture; Postural Recovery; Apparel Technology; Scapular Kinetics
Introduction
Daily activities that are unavoidable to many in the modern world, such as long commutes, hunching over computers and smart phones, and performing strenuous tasks at work often contribute to progressive poor posture, leading to chronic musculoskeletal complaints and poor ergonomics. Overhead athletes have particular challenges recovering from overuse injuries which can endanger their careers. Several studies have shown that the increasing usage of smart phones has exacerbated musculoskeletal problems by putting excessive pressure and tension on people’s necks and shoulders [1,2]. Additionally, many common occupational demands in fields such as parcel delivery, logistics, surgery, engineering and dentistry have a high prevalence of progressive neck and back pain symptoms. According to one study, up to eighty percent of people in the United States will experience a neck or back problem during their lifetime [3]. Neck, shoulder and back pain, commonly caused by progressive poor posture or overuse syndromes, can affect head-neck-scapular kinetics and muscular activities and greatly decrease a person's quality of life. However, the prevalence of posture related problems in the United States has consequences that reach far beyond physical discomfort. According to another study, Americans spend approximately 90 billion dollars on the diagnosis and management of back pain each year [4]. In addition to leading to neck and back conditions and their associated financial costs, poor posture can also influence mood, body balance, circulatory efficacy, breathing patterns [5,6], can cause imbalances in cortisol levels, and can lead to poor confidence, collaboration and decision making [7].
There is a strong relationship between neck and shoulder pain and the dysfunction of the scapula, which play a crucial role in providing both mobility and stability for the neck and shoulder region [8]. Poor scapular positioning can reduce the range of motion and strength of muscles over time, which can eventually lead to musculoskeletal disorders (MSDs) such as a rounded back (kyphosis), cervical neuropathy, and frozen shoulders. Proper scapular mechanics, on the other hand, allow the body to be correctly aligned and supported, and lead to healthier neck, back and shoulder biomechanics. The causal relationship between scapular dyskinesis, or an alteration in the normal position of the scapula, and neck and shoulder pain is not entirely clear. There is, however, some evidence that scapular dyskinesis, caused by anything from repetitive activity in athletes to hunching over a computer, could initially cause pain, and then become further exacerbated by the inhibitory responses of the body to that pain [8]. Regardless of the direction of the causal relationship, however, it is widely believed that clinicians should focus on scapula examination and rehabilitation in the treatment of neck and shoulder pain [8]. Because poor scapular positioning can lead to pain and a need for costly medical interventions over time, posture correcting devices that can prevent injury in the first place, such as back braces or taping, have important implications for decreasing the prevalence of back pain in the general population and its associated costs.
Posture correcting braces and taping methods have been shown to be effective in correcting posture and are widely used as affordable alternatives or supplements to more time consuming and costly treatments like physical therapy or orthopedic surgery. Studies have shown that subjects with pathologies such as shoulder impingement syndrome may show decreased scapular upward rotation and posterior tilt and increased scapular internal rotation [9]. One study of 30 subjects by Uhl et al. [10] demonstrated that wearing a scapular brace significantly increased participants’ posterior tilt and decreased their internal rotation, leading them to conclude that a scapular brace could improve scapular positioning both at rest and in motion. Another study by Cole et al. [11] similarly demonstrated that wearing a scapular brace immediately improved participants’ posture by decreasing forward shoulder tilt, or an imbalance in the muscles that upwardly and downwardly rotate the scapula. Additionally, Cole et al. [11] showed small but significant alterations in muscle activity while wearing the brace. An altered position of the scapula is associated with alterations in the electromyographic (EMG) activity of the muscles surrounding the scapula and glenohumeral joint, which can lead to tissue overload and injury [11]. Specifically, patients with overuse shoulder conditions have been shown to display decreased lower trapezius activity during shoulder motions [12], and studies have shown that irregular postures like Forward Head pose, Rounded Shoulder pose, or both, are related to increased upper trapezius activity [13]. Therefore, better posture is associated with both increased lower trapezius activity and decreased upper trapezius activity. In their study, Cole et al. [11] showed that wearing the brace increased participants’ lower trapezius EMG amplitude and that it decreased participants’ middle trapezius and upper trapezius EMG amplitude, indicating that participants’ posture had improved while wearing the brace. Similar results have been found by Selkowitz et al. [14] who showed that, in a sample of patients with shoulder impingement syndrome, or inflamed rotator cuff muscles, scapular taping resulted in decreased upper trapezius EMG amplitude and increased lower trapezius EMG amplitude in a reaching task. Significant evidence demonstrates, therefore, that various forms of posture correcting braces and taping can effectively alter participants’ scapular positioning and muscle activity surrounding the scapula, indicating improved posture.
Although traditional postural braces and taping methods have been shown to effectively correct posture by mechanically altering the scapula and affecting the surrounding muscle activity, they are limited in their ability to prevent the widespread development of musculoskeletal disorders in the general population. Back braces function by constricting body movement, forcing the body into the desired postural position. While constricting movement is not necessarily detrimental to the body or the development of better posture, such a confining garment may not be practical or comfortable for everyday use, and often lead to patient noncompliance and muscle weakness. Patient noncompliance has been shown to significantly decrease the treatment success of back braces. Rahmen et al. [15] examined the rates and consequences of noncompliance with back brace treatment for 34 scoliosis patients. They measured compliance electronically by using a temperature sensor embedded in the back brace. Their results showed that the noncompliance rate was much higher for patients whose condition did not progress, at 85 percent, when compared with the rate of noncompliance for patients whose condition did progress, at 62 percent. These results suggest that compliance with a brace treatment is crucial to the success of that treatment. Furthermore, their results indicate that most participants did not comply with their brace treatment as instructed, suggesting that noncompliance is a common phenomenon that should be addressed in future back treatment strategies.
In order to encourage the widespread use of a posture correcting device with the goal of reducing the costs of back, neck and shoulder pain for the greatest possible number of people, a device that is comfortable, practical and easy to wear while performing a variety of daily tasks would be most effective. The goal of the current study is to assess an innovative apparel technology by IFGFIT, a shirt with an integrated inner lining for posture restoration and recovery, and its effects on static scapular alignment and dynamic muscle activities. The FIT garment is a posture recovering shirt that allows for shoulder mobility, is breathable, is aesthetically pleasing to promote patient compliance, and is not compressive and uncomfortable to wear. The FIT tech garment contains technology that naturally pulls a wearer’s shoulders down and back, putting the wearer’s shoulders into proper alignment. Additionally, the garment acts as a feedback tool, so that when the wearer is in proper alignment, the tension in the shirt stops. This feedback trains the wearer to be in proper alignment, acting as a form of body and posture recovery. While wearing the FIT tech garment, shoulder scapular kinetics should improve instantly. By narrowing the distance between participants’ scapulae, the lumbar muscle activation level should increase, and the trapezius muscle activation level should decrease.
Materials and Methods
Subjects: A pilot sample of 21 volunteers was randomly selected to test the effectiveness of the FIT apparel technology. The pilot sample included 11 women and 10 men between the ages of 19 and 72. Prior to the study, each participant signed an informed consent document and provided demographic information including age, gender, and athlete status. Individuals who spent more than four days per week in the gym for over 30 minutes were categorized as recreational athletes. Of the pilot sample, 7 participants were listed as athletes, while 14 participants were not. The study was conducted in cities across the United States including Los Angeles, Boston, and New York.
Equipment: PPRTM apparel technology, designed by IFGFIT, consists of a mesh lining integrated into a lightweight, poly-blend grey crew neck garment. All participants were asked to wear the integrated garment during the study.
Surface electromyography (sEMG), a non-invasive technique for measuring muscle activity, sensors were directly attached to participants’ middle trapezius and lower erector spinae. sEMG sensors were used to measure the muscle activities while individuals were standing naturally and breathing normally. A MyoWareTMMuscle Sensor was used as a mobile electromyograph without filtering. Rectified EMG signals without hardware or software filtering were used when recording EMG voltages. As opposed to filtered EMG signals, which use low and high pass electrical filters to remove specific frequencies and reduce signal noise, rectified EMG signals lack frequency filtering and use only positive voltage values. These values are necessary to calculate the mean frequency of the signal later in the study (Figure 1).
Figure 1: FIT wearable Gray garment with sEMG sensors attached to the lumbar muscle.
The mean frequency and voltage of the signal were calculated using MatLab. The mobile sEMG was attached using 3M™ Red Dot™ monitoring electrodes with foam tape and sticky gel. Data was collected using an Adafruit Feather 32u4 Bluefruit LE and transmitted to MatLab using an attached HC-06 Bluetooth module. The circuit was powered by a 3.3v lithium polymer battery supplied by Adafruit. Mean frequency was calculated using the meanfreq() MatLab function and sampling rates dependent on individual measurement duration and samples collected.
Measurement: Scapular alignment of each participant at rest in standing position was recorded using the Lennie Test [16](Figure 3a-b). Scapular kinematics were determined for muscle activities of the middle trapezius and lower erector spinae using an sEMG (Figure 2a-c). Three electrodes were used for each muscle group. Two electrodes were placed at the middle and the end of the muscle while the third electrode was placed on the unaffected muscle groups as the reference node. All data was recorded with the subject in a neutral posture position. This position was determined by the subject’s rested standing position before and during the application of the PPRTM shirt.

Figure 2a: sEMG sensors were placed at the middle trapezius.

Figure 2b: sEMG sensors were placed at the lower erector spinae.

Figure 2c: Overall sEMG electrodes placement.
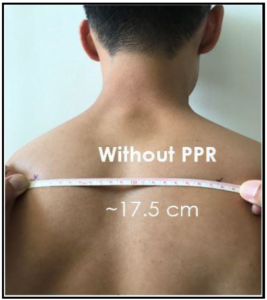
Figure 3a. Scapular positioning without FIT Garment.

Figure 3b: Scapular positioning with FIT Garment.
Mean voltage was used to indicate the difference in the mean power output by the muscles over the given time period. Additionally, mean frequency was used to calculate the change in muscle activation measured over samples per second. Mean frequency difference and mean voltage difference were determined by calculating the mean frequency and voltage of each patient’s data before and during the application of the shirt. The difference between the mean frequency and voltage before and during application of the shirt were then calculated to obtain an overall metric of change. The mean of this difference from each patient was then calculated to provide an average metric of change for all patients. As defined above, rectified EMG signals were collected using MatLab as continuous data during a 20-second interval and output voltages were adjusted based on the 3.3v input of the lithium battery.
Using the Lennie test [16], subject scapular alignment was evaluated while subjects were wearing the FIT shirt and then was compared to the scapular alignment of subjects previously recorded without the FIT shirt on. The muscle activity for both the middle trapezius and lower erector spinae muscle groups was recorded by sEMG over a 20-second interval before participants put on the FIT garment, and again while they were wearing the FIT garment. All sEMG measurements were transmitted via Bluetooth to a computer and analyzed using MatLab.
Results and Discussion
Results: A two-sample t-test found a significant effect of the FIT apparel tech on resting scapular position, t (40) = 3.87, p< .05, SD = 11.67mm. The t-test assumed normal distributions with unknown, but equal variances. Using a 95% confidence interval, individuals obtained a scapular positioning difference of between 6.64mm and 21.2mm, with a mean of 13.625mm. All subjects saw a notable improvement in their scapular positioning. One individual saw a 21.2mm change in the distance between scapula before and while wearing the FIT garment.
Two additional two-sample t-tests were performed to determine if the FIT shirt had improved scapular retraction based on gender or athletic training. Recreational athletes had a statistically significant increase in scapular retraction, t(19) = 3.521, p< .05, SD = 5.59mm. No statistical significance was found between gender and scapular retraction t(19) = 1.013, p> .05, SD = 7mm. Both the recreational athlete and gender equivalency t-test, (df = 19), assumed normal distributions with unknown, but equal variances. Additionally, no correlation (r = -.1024) was found between age of the participants and difference in scapular contraction.
A two-sample one-sided t-test was conducted to calculate the effect of the FIT garment on the EMG signals of each muscle group before and while wearing the FIT shirt. All t-tests assumed normal distributions with unknown, but equal variances. Difference between the mean voltage (p = .3928) and mean frequency (p = .3551) of the middle trapezius before and while wearing the FIT garment did not show statistical significance but did trend towards a difference. Analysis of EMG data found that the mean frequency difference of -.0235Hz and mean voltage difference of -.0539mV were lower in the mid trapezius after the application of the FIT shirt despite the lack of significance (Figure 4). Difference between the mean voltage (p = .1499) and mean frequency (p = .2425) of the erector spinae before and while wearing the FIT shirt did not show statistical significance either but did also trend towards a difference. EMG data also found that the mean frequency difference of .0314Hz and mean voltage difference of .1282mV were higher in the erector spinae while wearing the FIT garment (Figure 4).
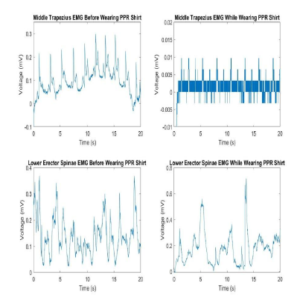 Figure 4: Subject sample showing lower mean frequencies and voltages in the middle trapezius and higher mean frequencies and voltages in the erector spinae while wearing the FIT shirt.
Figure 4: Subject sample showing lower mean frequencies and voltages in the middle trapezius and higher mean frequencies and voltages in the erector spinae while wearing the FIT shirt.
Discussion and Conclusion
The current study examined whether wearing the FIT apparel tech affected participants’ Scapular kinematics, specifically the ability to restore posture by altering their scapular positioning and muscle activity. To test this, the Lennie Test [16] was used to measure scapular alignment before and while participants wore the FIT shirt, and sEMG was used to measure muscle activity in the lower erector spinae and middle trapezius muscle groups before and while participants wore the FIT shirt. The results showed that while participants were wearing the shirt, their scapula were closer together, indicating that their scapular alignment had improved. Wearing the apparel did not, however, significantly affect sEMG muscle activity in the middle trapezius or in the lower erector spinae, although trends in the data did indicate that the middle trapezius muscles were less active, and the lower erector spinae muscles were more active while participants were wearing the apparel. Although not significant, the sEMG results trend towards improved spinal support while wearing the FIT shirt.
The scapular alignment results are consistent with our predictions for the current study and with previous literature that suggests that posture correcting devices can improve scapular alignment, leading to better posture [11]. Although the sEMG results did not find a significant effect of the FIT apparel tech on muscle activity, the trends in the data should be considered. The muscle activity results were trending in the direction of our prediction, meaning that there was a decrease in middle trapezius activity and an increase in lower erector spinae activity. The direction of these trends, although not significant, were consistent with the EMG findings of previous studies [11,14]. Since the EMG results trended in the direction of our hypothesis, one possible explanation for the lack of significance in the data could be a lack of statistical power, meaning that we did not have enough participants to find an effect of the shirt on muscle activity at this time.
Given these results, future research should test this apparel on larger samples to determine whether or not it alters muscle activity. Future research should also improve upon the equipment used and should use medical-grade EMG equipment or subdermal electrodes to produce better data and more accurate results. Gel-pad electrodes are able to reduce motion artifacts but may suffer in accuracy due to the micro-movements that a standing patient may undergo. This can be prevented through the use of subdermal electrodes, which are not affected by epidermal movement. Medical-grade EMG equipment are not without downsides. Though the advanced filtering methods of the medical-grade equipment may improve the accuracy of results, they may also remove outlying data that could change the results of the study.
Posture recovery apparel technology has not before been tested for its effects on scapular alignment and muscle activity and expands upon the previous back brace literature because it is comfortable, stylish for active wear, and less restrictive than traditional braces and compression shirts. The result that this active garment produced similar scapular alignment correction to more restrictive braces and compression shirts has implications for patient compliance. If more people are willing to wear this garment regularly, not just as a treatment for pain, but also as a preventative measure taken to avoid developing pain, the physical and financial costs of musculoskeletal pain and injury on society could be greatly reduced. The current study provides a basis for future exploration into the potential of posture restoring apparel technology to reduce pain and injury that results from progressive poor posture. Further research should be done on FIT apparel technology to better understand its potential for prolonged alteration in scapular kinematics and increased participant compliance compared with other traditional braces. For example, a longitudinal study using the FIT apparel could provide more insight into the long-term recovery benefits of wearing this garment and its effect on patient compliance over time.
References
- Jung SI, Lee NK, Kang KW, Kim K, Lee DY (2016) The effect of smartphone usage time on posture and respiratory function. Journal of Physical Therapy Science 28: 186-189.
- Cuddy A: Your iPhone Is Ruining Your Posture - and Your Mood. New York Times December 12, 2015.
- Rubin DI (2007) Epidemiology and risk factors for spine pain. Neurologic clinics 25: 353-371.
- Davis MA (2012) Where the United States spends its spine dollars: expenditures on different ambulatory services for the management of back and neck conditions. Spine 37: 1693.
- Harvard Medical school (2018, September). 3 surprising risks of poor posture Available at : [https://www.health.harvard.edu/staying-healthy/3-surprising-risks-of-poor-posture].
- Castaneda R: 10 Ways Poor Posture Can Harm Your Health.US News (2018).
- Cuddy AJC, Wilmuth CA, and Carney DR (2012) The Benefit of Power Posing Before a High-Stakes Social Evaluation. Harvard Business School Working Paper 13-027.
- Cools AM, Struyf F, Mey KD, Maenhout A, Castelein B, et al. (2014) Rehabilitation of scapular dyskinesis: From the office worker to the elite overhead athlete. British Journal of Sports Medicine 48: 692-697.
- Phadke V, Camargo PR, Ludewig PM (2009) Scapular and rotator cuff muscle activity during arm elevation: a review of normal function and alterations with shoulder impingement. Brazilian Journal of Physical Therapy 13: 1-9.
- Uhl TL, Kibler WB, Tripp BL, Spigelman TH, and McClelland RI (2006) Effects of S3 brace on scapular resting position and kinematics. Paper presented at: Annual Meeting of the American Orthopaedic Society for Sports Medicine.
- Cole AK, Mcgrath ML, Harrington SE, Padua DA, Rucinski TJ and Prentice WE (2013) Scapular Bracing and Alteration of Posture and Muscle Activity in Overhead Athletes With Poor Posture. Journal of Athletic Training 48: 12-24.
- Thigpen CA, Padua DA, Michener LA, Guskiewicz K, Giuliani C, et al. (2010) Head and Shoulder Posture Affect Scapular Mechanics and Muscle Activity in Overhead Tasks. Journal of Electromyography and Kinesiology 20: 701-709.
- Weon JH, Oh JS, Cynn HS, Kim YW, Kwon OY, et al. (2010) Influence of Forward Head Posture on Scapular Upward Rotators during Isometric Shoulder Flexion. Journal of Bodywork and Movement Therapies 14: 367-374.
- Selkowitz DM, Chaney C, Stuckey SJ, Vlad G (2007) The effects of scapular taping on the surface electromyographic signal amplitude of shoulder girdle muscles during upper extremity elevation in individuals with suspected shoulder impingement syndrome. Journal of orthopaedic& sports physical therapy 37: 694-702.
- Rahman T, Bowen JR, Takemitsu M, Scott C (2005) The Association Between Brace Compliance and Outcome for Patients With Idiopathic Scoliosis. Journal of Pediatric Orthopaedics 25: 420-422.
- Sobush DC, Simoneau GG, Dietz KE, Levene JA, Grossman RE, et al. (1996) The lennie test for measuring scapular position in healthy young adult females: a reliability and validity study. Journal of Orthopaedic& Sports Physical Therapy 23: 39-50.
Citation: Liu S, Bornstein J, Matsumura D, Liu S,Rahaman I,Li B, Liu M, Brien E (2019) The Effects of A Dynamic Apparel Technology on Scapular Kinematics and Muscle Activity. Adv Ortho and Sprts Med: AOASM-108.
