Concentration of Iodine in Iodized Common salt at Household Level and Associated Factors In Jabitehnan Woreda, West Gojjam Zone, North West, Ethiopia , 2015: A Cross-Sectional Study
Wubetu Woyraw1*, Getachew Hailu2, Getachew Mengistu3
1Department of Nutrition and Food Science, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
2Department of public health, school of Health Sciences, Bahirdar University, Bahirdar, Ethiopia
3Department of medical Laboratory science, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Received Date: 27 August, 2018; Accepted Date: 3 September, 2018; Published Date: 12 September, 2018
*Corresponding auth author: Wubetu woyraw, Department of Nutrition and Food Science, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia. Tel: +251918550243; Email: wubetu662@gmail.com
Citation: Woyraw W, Hailu G, Mengistu G (2018) Concentration of Iodine in Iodized Common salt at Household Level and Associated Factors In Jabitehnan Woreda, West Gojjam Zone, North West, Ethiopia, 2015: A Cross-Sectional Study. Adv Nutri and Food Scie: ANAFS-107.
Abstract
Background: Iodine deficiency leads to wide spectrums of health problems like abortion, stillbirth, mental retardation, physical incapability and deafness which are called iodine deficiency disorder. Universal salt iodization and iodine capsule supplementation are ways to prevent and eliminate iodine deficiency disorder. USI has preventive and corrective measure if all households consume adequately iodized salt in which iodine concentration of the salt ≥ 15PPM. The aim of this study was determining concentration of iodine in iodized common salt at household level and associated factors in Jabitehnan Woreda West Gojjam Zone, Ethiopia, 2015.
Methods: we conducted community based cross-sectional study design from September 15-23/2015. Multi-stage sampling technique was used to select 560 study participants. Data from households were collected using interview and measuring salted concentration using iodine concentration test kit. Epidata 3.1 and SPSS version 16 were used for data entry and data analysis respectively. Multivariable logistic regression was used to identify determinant factors for iodine concentration in iodized salt.
Result: The iodine content in the salt samples collected from 48.3% of the households was adequate i.e., ≥15 ppm. Duration of salt storage (AOR=7.424(1.733-31.798)), packaging material (AOR=0.024(0.009-0.064)) and salt container (AOR=39.84(13.473-117.841)) were significantly associated with iodine concentration in iodized salt.
Conclusion: The concentration of iodine in iodized salt was not adequate as compared to the daily requirements of household member recommended by WHO to prevented iodine deficiency disorder. Place of storage, having cover on the salt container, using salt packed with plastic material and short-term storage of salt at the household level are factors associated with concentration of iodine. Nutrition education and counselling about storage, duration, and volatility of iodized salt at household level should be given. Increasing awareness of females who are responsible for handling and utilization of iodized salt at household.
Keyword: Concentration; Iodine; Iodized Salt;
Introduction
Iodine deficiency disorder refers to a spectrum of health consequence resulting from inadequate intake of iodine source foods. Iodine deficiency leads to wide spectrums of health problems like abortion, stillbirth, mental retardation, physical incapability and deafness which is called iodine deficiency disorder. Taking low amounts of iodine in the diet i.e., less than 110-290 microgram per day based on a gender and age may lead to insufficient production of thyroid hormone which is the cause of iodine deficiency disorder [1].
Mental retardation and brain damage are result of IDD which can be easily prevented. Preventing IDD is a more superior approach than treatment as there are non- reversible consequences following treatment(1). Sever IDD which results cretinism [2], still birth and miscarriage in 5-15% of the population can be announced as sever if 30% and/or of the population is affected by goiter [3]. Mild and moderate IDD can affect the academic performance of the population [3]. As different study showed in goiter endemic areas reproductive failure which is result IDD can be corrected by iodine supplementation and salt iodization strategies [2]. Globally greater than two billion population, are estimated to be at risk of IDD. In Africa two hundred sixty billion population, are at risk of developing IDD [4]. In Ethiopia as survey conducted by EHNRI in 2005, shows the goiter prevalence is 40% in children and 36% in mothers. USI has preventive and corrective measure if all households consume adequately iodized salt in which iodine concentration of the salt ≥ 15PPM. There are two methods to assess the achievement of salt iodization. The first one is ≥90% of households should consume adequately iodized salt (≥ 15PPM).
According to study conducted on adequately iodized salt consumption of households in Uganda, Ghana, South Sudan, and Somalia is 96%, 75.6%, 72.9% and 6.7% respectively [7-10]. In Ethiopia 15.4% of population used adequately iodized salt which varies 6%-40% across regional states. The national iodine concentration in iodized salt estimated about 11.2% 0 ppm, 34.9% <15 ppm and 53.9% >15 ppm whereas the concentration in Amhara region is reported as 7.4% 0 ppm,40.2% < 15 ppm and 52.5% >15 ppm which is below standard [6].
Even if government plans to achieve the rural Ethiopian communities should access adequately iodized salt by 2015 by means USI, still the concentration of iodine in iodized salt is low It is critical to have an accurate estimate of the losses in iodine prior to consumption, so that the producers may compensate for the losses by the addition of appropriate iodine during production. We undertook a study to determine concentration of iodine in iodized common salt at household level and its associated factors using quality assured test methods in rural Jabitehnan District.
Methods
Study Subjects: A community based cross-sectional study design was conducted during September 15-23/2015 in 37 randomly selected rural and 2 urban kebeles of Jabitehnan, district to determine concentration of iodine in table salt and factors affecting concentration of iodine among households. Five hundred sixty households were included in the study, which is determined using a single proportion formula by taking (Prevalence (P) = 33% (19), Za/2=1.96 at 95 % confidence interval (z value at alpha =0.05, margin of error (d) = 0.05) and taking 10% for non –response rate. The sampling technique used in this study was multi-stage sampling technique. E i g h t kebeles was selected from the total 39 kebels in the district and then the total sample size was allocated proportionally to each selected kebeles. Then households were selected using systematic random sampling techniques (Figure 1).
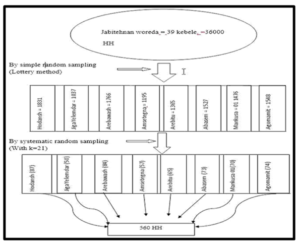
Figure 1: Schematic presentation of sampling procedure and technique for assessment of the concentration of iodine in iodized common salt at household level and its associated factors in Jabitehnan Woreda, West Gojjam Zone, North West Ethiopia, 2015.
N= 36000 household
P=0.33
n= (zα/2)2*p (1-p)
D2
Where n=sample size, Zα/2=critical value, P=prevalence, D= marginal error n= sample size, N=total population
n= (1.96)2 x 0.33(1-0.33) =340, non-response rate (10%) + n = 373 (0.05)2(0.05)2
Adding design effect (1.5) the total sample size was 560.
Operational Definitions: Adequate concentration: Household those who have >15 ppm iodine concentration in iodized salt Longer storage time: Participants who store the purchased salt for more than two months. Short storage time: those who stored for less than two months. Improper practice: any single practice that might result in the reduction of salt iodine content.
Data Collection Procedures: Data collection: questionnaire was held with face to face exit interview by pre-test structured questionnaire. The actual data collection was started after two days of training on data collection tool and Socio- Demographic characteristics such as age, religion, education status and ethnicity, place of storage, materials of storage and time spend in store place were collected on voluntary base using codes that maintain privacy of study participants.
Materials for Sample Collection and Procedures of Testing: Materials used for testing were MBIKITS salt test kit which contains small cup, two 10 ml test solutions, 10 ml recheck solution and color chart.
Procedure used: Fill the small cup with salt and make the surface flat. Then add two drops of test solution after shaking. Then wait for one minute and compare the color of salt with color chart. If no color appears add up to five drops of recheck solution.
Data Processing and Analysis: After data was collected it was entered into Epi data version 3.1and exported to SPSS version 16 then data was analyzed using SPSS version 16. Descriptive statistical analysis was performed and results were presented using tables and graphs. In order to assess the relationship of independent variable to dependent variable, logistic regression was used. Out of variables entered in to bivariate logistic regression, those with p-value less than 0.2 were again taken into multivariate logistic regression analysis with p –value < 0.05 and CI 95%. Odds ratio was used to assess the strength of association. Model fitness was tested using Hosmer and Lemeshow test at p>0.05 and the result of the regression analysis shows the model fits with the predictors (P=0.367).
Ethical Consideration: We obtained ethical clearance from debremarkos university ethical clearance committee. Letter was also obtained from Jabitehnan Woreda health office. Each participant was informed orally for the purpose of study and also voluntarism of participation so that they had full of right to withdraw from the study at any time.
Results
Socio-Demographic Characteristics: Out of 560 households 514 female and 35 male respondents were interviewed which gave 98% response rate. The mean age of the respondents was 38.2±8.54 years, ranging from 21-67 years. The majority (96%) of respondents was orthodox Christian by religion, 70.15 were married and 86.3% were unable to read and write (Table 1).
| Variables | Frequency | Percent |
| Age (in year) | ||
| 15-29 | 97 | 17.7 |
| 30-44 | 330 | 60.1 |
| ≥45 | 122 | 22.2 |
| Total | 549 | 100 |
| Sex | ||
| Male | 35 | 6.4 |
| Female | 514 | 93.6 |
| Total | 549 | 100 |
| Religion | ||
| Orthodox Christian | 527 | 96 |
| Muslim | 20 | 3.6 |
| Protestant | 1 | 0.2 |
| Catholic | 1 | 0.2 |
| Total | 549 | 100 |
| Marital status | ||
| Married | 385 | 70.1 |
| Single | 23 | 4.2 |
| Divorced | 72 | 13.1 |
| Widowed | 69 | 12.6 |
| Total | 549 | 100 |
| Educational status | ||
| Unable to read and write | 474 | 86.3 |
| Able to read and write | 75 | 13.7 |
| Total | 549 | 100 |
Concentration of Iodine in Iodized Salt at Household Level: The iodine content in the samples salt collected from 48.3% of the households were adequate i.e., ≥15 ppm. Around 50% of the respondents were use salt with plastic package, out of which 99.2% was adequately iodized. Forty three percent of the households got salt from weekly market of which 38.2% was adequately iodized. Nearly half of salt containers (56.5%) had a cover from which, 76.7% was adequately iodized. Thirty-nine percent of respondents exposed their salt to fire, 20.2% stored the salt in dry places and 16.9% stored for more than two months after purchase (Table 2).
|
Variables |
Frequency |
Percent |
|
|
Result of test kit |
>15ppm | 265 | 48.3 |
| 0-15ppm | 189 | 34.4 | |
| 0ppm | 95 | 17.3 | |
| Total | 549 | 100 | |
|
From where you buy salt |
Shop around the village | 99 | 18 |
| Town near the village | 201 | 36.6 | |
| Whole seller in the district | 11 | 2 | |
| Weekly market | 238 | 43.4 | |
| Total | 549 | 100 | |
|
Duration of salt storage Level |
< 2 month | 456 | 83.1 |
| ≥2 month | 93 | 16.9 | |
| Total | 549 | 100 | |
|
Salt container |
Container with cover | 310 | 56.5 |
| Container without cover | 239 | 43.5 | |
| Total | 549 | 100 | |
|
Amount of salt you buy at o |
<1 kg | 212 | 38.6 |
| 1-5kg | 281 | 51.2 | |
| >5kg | 56 | 10.2 | |
| Total | 549 | 100 | |
|
Salt storage place |
Dry place | 111 | 20.2 |
| Moist area | 223 | 40.6 | |
| Near to fire | 215 | 39.2 | |
| Total | 549 | 100 | |
| Availability of salt | Always avail | 549 | 100 |
|
How you by salt |
Loose | 293 | 53.4 |
| Packed with plastic or other | 256 | 46.6 | |
| Total | 549 | 100 | |
Factors Associated with the Concentration of Iodine in Iodized Salt at Household Level: Shorter duration of storage, place of storage, having a cover on the salt containers, using salt Packed with plastic material, buying salt from whole seller, sex and marital status were factors associated with the concentration of iodine in iodized salt in the bivariate logistic regression. However, in the multivariable logistic regression, only duration of salt storage, packaging material and salt container were independently associated with iodine concentration in salt in iodized salt The odds of being ≥15ppm are increased by a factor of 7.4 if the salt is stored for <2 month rather than storing for ≥2 month after controlling the other variables in the model. Households who used container with cover for salt storage were 38.8 times more likely to have adequately iodized salt compared to salts stored in container without cover (Table 3).
|
Variable
|
Concentration of iodine in iodized |
COR( 95.0% CI for COR) |
AOR(95.0% CI for AOR |
||
| <15PPM | ≥15PPM | ||||
| Duration of salt storage at household | < 2 month | 202 | 254 | 9.374(4.865-18.062) | 7.424(1.733-31.798) |
| ≥2 month | 82 | 11 | 1 | 1 | |
| How you buy salt | Loose | 245 | 47 | 0.035(0.022-0.056) | 0.024(0.009-0.064) |
| Packed with plastic or other material | 39 | 218 | 1 | 1 | |
| Salt container | Container with cover | 72 | 238 | 25.955(16.069-41.923) | 39.845(13.473-117.841) |
| Container without cover | 212 | 27 | 1 | 1 | |
Discussion
Rapid test kits were used for the assessment of iodine levels in the household salt samples because it gives reliable results immediately and this intern helps in the recommendation of iodine loss to those manufactures and aware the community by giving valuable information about iodine contents of the salt. According to different validation studies it ranges from 93.3%-- 93.3%but specificity varies with in single and multiple observation. The result of this study showed that 48.3% of households have iodized salt with concentration of iodine is ≥ 15PPM which is lower than the WHO’S recommendation [7]. But the result is higher than researches done in Gondar town and EDHS 2011 [6,8].This may be due to that Ethiopian government with ministry of health were strive to achieve universal salt iodization goals by implementing different strategies of fortification of salt, proper handling and utilization in the last few years. But, the prevalence of adequately concentrated iodine in iodized salt is law when compared to study conducted in Uganda, Ghana, south Sudan [9-11] therefore well-coordinated implementation strategy still needed to increase concentration of iodine in iodized salt in the study area. Concentration of iodine in iodized salt is independently associated with length of time that the salt stored in the house for consumption. The odds of being ≥15ppm are increased by a factor of 7.4 if the salt is stored for <2 month rather than storing for ≥2 month controlling the other variables in the model, which have comparable result study conducted in Gondar town [8]. Eighty-three percent of respondents store their salt for short period of time. Among them 55.7% households have adequate concentration of iodine in their iodized salt which is better than study in Gondar [8]. This may be due to the natural characteristics of iodine i.e. it’s easily volatility when exposed to humid area, moisture, light, during production. Distribution and households. This study revealed that buying packed salt and storing salt in container with cover is independently associated with iodine concentration in iodized salt. The multivariable analysis result indicates that the odds of being ≥15ppm is reduced by a factor of 0.024 in not packed salt compared to packed salt. Households who used container with cover for salt storage were 38 times more likely to have adequate concentration of iodine iodized salt compared to salts stored in container without cover, which is similar to study done in Gondar town [8] and a cross sectional study in Rural communities in Laelay Maychew District [12]. This is due to the reason that iodine can easily diffuse in the atmosphere.
Packaging affected the levels of moisture contained in the salt. In open containers the absorbed and condensed moisture was retained and contributed to the instability of iodine. The results indicate that the control of moisture content on iodized salt throughout the manufacturing and distribution or by improved processing and better packing of iodized salt is critical to the stability of the added iodine .In order to make allowances for the probable losses of iodine, countries must determine iodine losses from local iodized salt at household level, because it is greatly affected by salt source, and packing and processing technology.
Conclusion
The concentration of iodine in iodized salt was not adequate as compared to the daily requirements of household member recommended by WHO to prevent iodine deficiency disorder. Place of storage, having cover on the salt container, using salt packed with plastic material and short-term storage of salt at the household level are factors associated with concentration of iodine. Responsible bodies like Woreda health extensions, Woreda health office, and health centre professionals should deliver continuous nutrition education and counselling about storage, duration and volatility of iodine in iodized salt at house hold level. Increasing awareness of females who are responsible for handling and utilization of iodized salt at household.
Abbreviations and Acronyms AOR : Adjusted Odd Ratio; CIF : Central Iodization Facility; COR : Crude Odd Ratio; EDHS : Ethiopian Demographic Health Survey; HH : House Hold; ICCIDD : International Council for Control of Iodine Deficiency Disorder; IDD : Iodine Deficiency Disorder; PPM : Parts Per Million; UNICEF : United Nation Children Fund; USI : Universal Salt Iodization; WHO : World Health Organization
Declarations
- Ethics approval and consent to participate: We obtained ethical clearance from debremarkos university ethical clearance committee. Letter was also obtained from Jabitehnan Woreda health office. Each participant was informed orally for the purpose of study and also voluntarism of participation so that they had full of right to withdraw from the study at any time.
- Consent for publication: Not applicable
- Availability of data and material: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
- Conflict of interests: The authors have declared that no competing interests exist.
- Funding: No funding was obtained for this study.
- Author Contributions
- Conceptualization: Formal analysis: WW GH GM. Development or design of methodology:
- GH GM. Entering data into computer software: WW GH GM. Supervision: WW GH GM Validation: GH GM. writing original draft: WW GH GM. Writing review & editing: WW GH GM. All authors read and approved the final manuscript.
Acknowledgements: We would like to thank Debre Markos University College of health science for providing ethical clearance, data collectors, supervisor and study participants.
References
- Secretariat W, Andersson M, De Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public health nutrition 10: 1606-16011.
- Abuye C, Berhane Y (2007) The goitre rate, its association with reproductive failure, and the knowledge of iodine deficiency disorders (IDD) among women in Ethiopia: Cross-section community based study. BMC Public Health 7: 316.
- Fisch A, Pichard E, Prazuck T, Sebbag R, Torres G, et al. (1993) A new approach to combatting iodine deficiency in developing countries: the controlled release of iodine in water by a silicone elastomer. American journal of public health 83: 540-545.
- Krämer M (2017) Nutrition and Child Development in Low-and Middle-Income Countries-Evaluation of Three Micronutrient Interventions.
- Diosady LL, Alberti JO, Mannar MGV, FitzGerald S (2012) Stability of iodine in iodized salt. I odine nutrition and universal salt iodisation: landscape analysis.
- Cs. Ethiopian demographic health survey. 2011.
- Organization WH (2001) WHO. International Council for Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. A guide programmed managers, Geneva, Switzerland, WHO, Department of Nutrition for Health and Development; 2001. WHO/NHD/01.1.
- Gebremariam HG, Yesuf ME, Koye DN (2013) Availability of adequately iodized salt at household level and associated factors in Gondar town, Northwest Ethiopia. ISRN Public Health 2013.
- Mutwakel Gaffar A, Salih Mahfouz M (2011) Peace impact on health: population access to iodized salt in south Sudan in postconflict period. Croatian medical journal 52: 178-182.
- Buxton C, Baguune B (2012) Knowledge and practices of people in BiaDistrict, Ghana with regard to iodine deficiency disorders and intake of iodized salt. Arch public health 70: 5.
- IOM MORCMI (2006) Uganda Demographic Health Survey.
- Gidey B, Alemu K, Atnafu A, Kifle M, Tefera Y, et al. (2015) Availability of adequate iodized salt at household level and associated factors in rural communities in Laelay Maychew District, Northern Ethiopia: a cross sectional study. Journal of Nutrition and Health Sciences 2: 1.
